In What Culture Are Older People Sometimes Afforded Special Status
In What Culture Are Older People Sometimes Afforded Special Status
Physical Development in Late Adulthood
The aging process often results in a loss of memory, deteriorated intellectual function, decreased mobility, and higher rates of disease.
Learning Objectives
Review the physical and neurological changes characteristic of late adulthood
Key Takeaways
Key Points
- During late adulthood the skin continues to lose elasticity, reaction time slows further, muscle strength and mobility diminishes, hearing and vision decline, and the immune system weakens.
- The aging process generally results in changes and lower functioning in the brain, leading to problems like decreased intellectual function and neurodegenerative diseases such as Alzheimer's.
- Many of the changes in the bodies and minds of older adults are due in part to a reduction in the size of the brain as well as loss of brain plasticity.
- Memory degenerates in old age, so older adults have a harder time remembering and attending to information. In general, an older person's procedural memory tends to remain stable, while working memory declines.
Key Terms
- cerebellum: Part of the hindbrain in vertebrates; in humans it lies between the brainstem and the cerebrum and plays an important role in sensory perception, motor output, balance, and posture.
- Alzheimer's disease: A disorder involving loss of mental functions resulting from brain-tissue changes; a form of senile dementia.
- corpus callosum: In mammals, a broad band of nerve fibers that connects the left and right hemispheres of the brain.
- neurodegenerative: Of, pertaining to, or resulting in the progressive loss of nerve cells and of neurologic function.
Physical Changes
Late adulthood is the stage of life from the 60s onward; it constitutes the last stage of physical change. Average life expectancy in the United States is around 80 years; however, this varies greatly based on factors such as socioeconomic status, region, and access to medical care. In general, women tend to live longer than men by an average of five years. During late adulthood the skin continues to lose elasticity, reaction time slows further, and muscle strength diminishes. Hearing and vision—so sharp in our twenties—decline significantly; cataracts, or cloudy areas of the eyes that result in vision loss, are frequent. The other senses, such as taste, touch, and smell, are also less sensitive than they were in earlier years. The immune system is weakened, and many older people are more susceptible to illness, cancer, diabetes, and other ailments. Cardiovascular and respiratory problems become more common in old age. Seniors also experience a decrease in physical mobility and a loss of balance, which can result in falls and injuries.
Changes in the Brain
The aging process generally results in changes and lower functioning in the brain, leading to problems like memory loss and decreased intellectual function. Age is a major risk factor for most common neurodegenerative diseases, including mild cognitive impairment, Alzheimer's disease, cerebrovascular disease, Parkinson's disease, and Lou Gehrig's disease.
While a great deal of research has focused on diseases of aging, there are only a few informative studies on the molecular biology of the aging brain. Many molecular changes are due in part to a reduction in the size of the brain, as well as loss of brain plasticity. Brain plasticity is the brain's ability to change structure and function. The brain's main function is to decide what information is worth keeping and what is not; if there is an action or a thought that a person is not using, the brain will eliminate space for it.
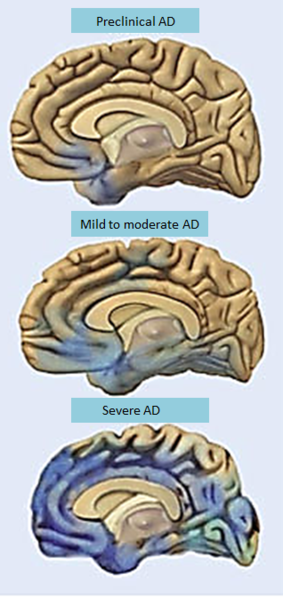
Photos depicting the progression of Alzheimer's disease: Alzheimer's disease (AD) is a neurodegenerative disease and is the most common form of dementia in older adults.
Brain size and composition change along with brain function. Computed tomography (CT) studies have found that the cerebral ventricles expand as a function of age in a process known as ventriculomegaly. More recent MRI studies have reported age-related regional decreases in cerebral volume. The brain begins to lose neurons in later adult years; the loss of neurons within the cerebral cortex occurs at different rates, with some areas losing neurons more quickly than others. The frontal lobe (which is responsible for the integration of information, judgement, and reflective thought) and corpus callosum tend to lose neurons faster than other areas, such as the temporal and occipital lobes. The cerebellum, which is responsible for balance and coordination, eventually loses about 25 percent of its neurons as well.
Changes in Memory
Memory also degenerates with age, and older adults tend to have a harder time remembering and attending to information. In general, an older person's procedural memory stays the same, while working memory declines. Procedural memory is memory for the performance of particular types of action; it guides the processes we perform and most frequently resides below the level of conscious awareness. In contrast, working memory is the system that actively holds multiple pieces of transitory information in the mind where they can be manipulated. The reduced capacity of the working memory becomes evident when tasks are especially complex. Semantic memory is the memory of understanding things, of the meaning of things and events, and other concept-based knowledge. This type of memory underlies the conscious recollection of factual information and general knowledge about the world, and remains relatively stable throughout life.
Cognitive Development in Late Adulthood
Cognitive abilities such as memory may see a decline in late adulthood.
Learning Objectives
Review the cognitive changes characteristic of late adulthood
Key Takeaways
Key Points
- During old age, a general decline in memory is very common, due to the decrease in speed of encoding, storage, and retrieval of memory.
- Neurocognitive disorder, formerly called dementia, is a broad category of brain diseases that cause a gradual long-term decrease in the ability to think and remember.
- There is no cure for neurocognitive disorder, but there are many strategies to improve quality of life for people with this disorder, such as daily exercise programs and cognitive or behavioral therapies.
Key Terms
- dementia: A broad category of brain diseases that cause a long-term decrease in the ability to think and remember to the extent that a person's daily functioning is affected.
As an individual ages into late adulthood, psychological and cognitive changes can sometimes occur. A general decline in memory is very common, due to the decrease in speed of encoding, storage, and retrieval of information. This can cause problems with short-term memory retention and with the ability to learn new information. In most cases, this absent-mindedness should be considered a natural part of growing older rather than a psychological or neurological disorder.

Intelligence: Cognitive ability changes over the course of a person's lifespan, but keeping the mind engaged and active is the best way to keep thinking sharp.
Distinct from a normal decline in memory is dementia, a broad category of brain diseases that cause a gradual long-term decrease in the ability to think and remember to the extent that a person's daily functioning is affected. While the term "dementia" is still often used in lay situations, in the DSM-5 it has been renamed "neurocognitive disorder," with various degrees of severity.
Alzheimer's disease is the most common type of neurocognitive disorder, accounting for 50% to 70% of cases. Neurocognitive disorders most commonly affect memory, visual-spatial ability, language, attention, and executive function (e.g., judgment and problem-solving). Most of these disorders are slow and progressive; by the time a person shows signs of the disease, the changes in their brain have already been happening for a long time. About 10% of people with dementia have what is known as mixed dementia, which is usually a combination of Alzheimer's disease and another type of dementia.
There is no cure for dementia, but for people who suffer from these disorders and for their caregivers, many measures can be taken to improve their lives. These can include education and support for the caregiver and daily exercise programs or cognitive or behavioral therapies for the person with the disorder.
Socioemotional Development in Late Adulthood
Growing older means confronting many psychological, emotional, and social issues that come with entering the last phase of life.
Learning Objectives
Review the socioemotional changes and crises characteristic of late adulthood
Key Takeaways
Key Points
- As people age, they become more dependent on others. Older adults may struggle with feelings of guilt, shame, or depression because of their increased dependency, especially in societies where the elderly are viewed as a burden.
- Many older adults contend with feelings of loneliness and isolation as their loved ones pass away, which can negatively impact their health and well-being. Staying active and involved in life can help to counteract these challenges.
- According to Erikson, the final stage of life is marked by a crisis over integrity vs. despair. People who believe they have had a positive impact on the world feel a sense of integrity, while those who feel they have not measured up to certain standards develop a sense of despair.
- According to Elisabeth Kübler-Ross, people go through five distinct stages of grief upon dealing with death and dying: denial, anger, bargaining, depression, and acceptance.
Key Terms
- socioemotional selectivity theory: A life-span theory of motivation which maintains that as time horizons shrink, as they typically do with age, people become increasingly selective, investing greater resources in emotionally meaningful goals and activities.
- hospice: The provision of palliative care for terminally ill patients, either at a specialized facility or at a residence, along with support for the family; typically refrains from taking extraordinary measures to prolong life.
As people approach the end of life, changes occur and special challenges arise. Growing older means confronting many psychological, emotional, and social issues that come with entering the last phase of life.
Increased Dependency
As people age, they become more dependent on others. Many elderly people need assistance in meeting daily needs as they age, and over time they may become dependent on caregivers such as family members, relatives, friends, health professionals, or employees of senior housing or nursing care. Many older adults spend their later years in assisted living facilities or nursing homes, which can have social and emotional impacts on their well-being. Older adults may struggle with feelings of guilt, shame, or depression because of their increased dependency, especially in societies where caring for the elderly is viewed as a burden. If an elderly person has to move away from friends, community, their home, or other familiar aspects of their life in order to enter a nursing home, they may experience isolation, depression, or loneliness.
Increased dependency can also put older adults at risk of elder abuse. This kind of abuse occurs when a caretaker intentionally deprives an older person of care or harms the person in their charge. The elderly may be subject to many different types of abuse, including physical, emotional, or psychological. Approximately one in ten older adults report being abused, and this number rises in the cases of dementia or physical limitations.
Despite the increasing physical challenges of old age, many new assistive devices made especially for the home have enabled more old people to care for themselves and accomplish activities of daily living (ADL). Some examples of devices are a medical alert and safety system, shower seat (preventing the person from getting tired in the shower and falling), bed cane (offering support to those with unsteadiness getting in and out of bed), and ADL cuff (used with eating utensils for people with paralysis or hand weakness). Advances in this kind of technology offer increasing options for the elderly to continue functioning independently later into their lives.
Loneliness and Connection
A central aspect of positive aging is believed to be social connectedness and social support. As we get older, socioemotional selectivity theory suggests that our social support and friendships dwindle in number, but remain as close as, if not closer than, in our earlier years (Carstensen, 1992). Many older adults contend with feelings of loneliness as their loves ones, partners, or friends pass away or as their children or other family members move away and live their own lives. Loneliness and isolation can have detrimental effects on health and psychological well-being. However, many adults counteract loneliness by having active social lives, living in retirement communities, or participating in positive hobbies. Staying active and involved in life counteracts loneliness and helps increase feelings of self-esteem and self-worth.

Social relationships in old age: Research has shown that social support is important as we age, especially as loss and death become more common.
Erikson: Integrity vs. Despair
As people enter the final stages of life, they have what Erik Erikson described as a crisis over integrity versus despair. In other words, they review the events of their lives and try to come to terms with the mark (or lack thereof) that they have made on the world. People who believe they have had a positive impact on the world through their contributions live the end of life with a sense of integrity. Those who feel they have not measured up to certain standards—either their own or others'—develop a sense of despair.
Confronting Death
People perceive death, whether their own or that of others, based on the values of their culture. People in the United States tend to have strong resistance to the idea of their own death and strong emotional reactions of loss to the death of loved ones. Viewing death as a loss, as opposed to a natural or tranquil transition, is often considered normal in the United States. Elisabeth Kübler-Ross (1969), who worked with the founders of hospice care, described in her theory of grief the process of an individual accepting their own death. She proposed five stages of grief in what became known as the Kübler-Ross model: denial, anger, bargaining, depression, and acceptance.
- Denial: People believe there must be some mistake. They pretend death isn't happening, perhaps live life as if nothing is wrong, or even tell people things are fine. Underneath this facade, however, is a great deal of fear and other emotions.
- Anger: After people start to realize death is imminent, they become angry. They believe life is unfair and usually blame others (such as a higher power or doctors) for the state of being they are experiencing.
- Bargaining: Once anger subsides, fear sets in again. Now, however, people plead with life or a higher power to give them more time, to let them accomplish just one more goal, or for some other request.
- Depression: The realization that death is near sets in, and people become extremely sad. They may isolate themselves, contemplate suicide, or otherwise refuse to live life. Motivation is gone and the will to live disappears.
- Acceptance: People realize that all forms of life, including the self, come to an end, and they accept that life is ending. They make peace with others around them, and they make the most of the time they have remaining.
While most individuals experience these stages, not all people go through every stage. The stages are not necessarily linear, and may occur in different orders or reoccur throughout the grief process. Some psychologists believe that the more a dying person fights death, the more likely they are to remain stuck in the denial phase, making it difficult for the dying person to face death with dignity. However, other psychologists believe that not facing death until the very end is an adaptive coping mechanism for some people.
Whether due to illness or old age, not everyone facing death or the loss of a loved one experiences the negative emotions outlined in the Kübler-Ross model (Nolen-Hoeksema & Larson, 1999). For example, research suggests that people with religious or spiritual beliefs are better able to cope with death because of their belief in an afterlife and because of social support from religious or spiritual associations (Hood, Spilka, Hunsberger, & Corsuch, 1996; McIntosh, Silver, & Wortman, 1993; Paloutzian, 1996; Samarel, 1991; Wortman & Park, 2008).
How Culture and Society Impact the Elderly
Depending on culture, aging can be seen as an undesirable phenomenon or as an accumulation of wisdom and status.
Learning Objectives
Analyze the effects of societal perception on treatment of the elderly
Key Takeaways
Key Points
- How people view and perceive the aging process varies greatly from culture to culture.
- Ageism is a common form of discrimination in the United States and other societies that includes negative views and stereotypes about the elderly. This type of discrimination can have a significant negative impact on the care and well-being of elderly people.
- Traditionally, elder care has been the responsibility of family members and was provided within an extended-family home. However, increasingly in modern societies, elder care is being provided by state or charitable institutions.
- Assisted living facilities allow the elderly to keep a sense of independence while providing them with care and supervision necessary to stay safe.
- While countries like the United States and Japan focus more on independent care, Indian culture places greater emphasis on respect and family care for the elderly.
- People also perceive death based on the values of their culture. In the United States, it is fairly normal to view death as a loss and something to be feared, as opposed to a natural or tranquil transition.
Key Terms
- culture: The beliefs, values, behavior, and material objects that constitute a people's way of life.
- prejudice: An adverse judgment or opinion formed beforehand or without knowledge of the facts.
- self-fulfilling prophecy: A prediction that, by being voiced, causes itself to come true.
How people view and perceive the aging process varies greatly from culture to culture. Depending on cultural norms, beliefs, and standards, aging can be seen as an undesirable phenomenon, reducing beauty and bringing one closer to death, or as an accumulation of wisdom and status worthy of respect. In some cases, numerical age is important (whether good or bad), whereas in other cases the stage in life that one has reached (adulthood, independence, marriage, retirement, career success) is deemed more important than numerical age.

Cultural views on aging: Depending on the culture, aging can be seen as an undesirable phenomenon or as an accumulation of wisdom and respect.
Aging and Ageism
Ageism (also spelled "agism") involves stereotyping and discriminating against individuals or groups on the basis of their age. The term was coined in 1969 by Robert Neil Butler to describe discrimination against seniors, and it operates similarly to the way that sexism and racism operate. Butler defined ageism as a combination of three connected elements: prejudicial attitudes toward older people, old age, and the aging process; discriminatory practices against older people; and institutional practices and policies that perpetuate stereotypes about elderly people.
Research on age-related attitudes in the United States consistently finds that negative attitudes exceed positive attitudes toward older people because of their looks and behavior. In his study Aging and Old Age, Posner (1997) discovered "resentment and disdain of older people" in American society. The stereotypes, discrimination, and devaluing of the elderly seen in ageism can have significant effects on the elderly, affecting their self-esteem, emotional well-being, and behavior. After repeatedly hearing the stereotype that older people are useless, older people may begin to feel like dependent, non-contributing members of society. They may start to perceive themselves in the same ways that others in society see them. Studies have also specifically shown that when older people hear these stereotypes about their supposed incompetence and uselessness, they perform worse on measures of competence and memory; in effect, these stereotypes become a self-fulfilling prophecy.
According to Cox, Abramson, Devine, and Hollon (2012), old age is a risk factor for depression caused by such prejudice. When people are prejudiced against the elderly and then become old themselves, their anti-elderly prejudice turns inward, causing depression. Research has found that people who hold more ageist attitudes or negative age-related stereotypes are more likely to face higher rates of depression as they get older. Old-age depression results in the over-65 population having one of the highest rates of suicide.
Eldercare
The form of eldercare provided varies greatly among countries and is changing rapidly. Even within the same country, regional differences exist with respect to care for the elderly, often depending on the resources available in a given community or area. However, it has been observed that globally the elderly consume the most health expenditures out of any other age group. Traditionally, eldercare was the responsibility of family members and was provided within an extended family home. Increasingly in U.S. society, eldercare is being provided by state or charitable institutions.
In developed countries such as the United States, nearly one million elderly citizens are helped by assisted living facilities. These facilities allow the elderly to keep a sense of independence while providing them with the care and supervision necessary to stay safe. Other elderly people are cared for by members of their family; however, eldercare in the United States is often viewed as a burden by family members who are busy living their own lives, making assisted living and respite-care facilities a commonly chosen option.
Cultural Views on Aging and Death
While countries like the United States and Japan focus more on independent care, Indian culture places greater emphasis on respect and family care for the elderly. In contrast to the United States, many countries view elderly citizens, especially men, in very high regard. Traditional values demand honor and respect for older people, who are considered to be wiser from experience. In China, several studies have noted the attitude of filial piety, or deference and respect to one's parents and ancestors in all things, as defining all other virtues.
People also perceive death, whether their own or that of others, based on the values of their culture. People in the United States tend to have strong resistance to the idea of their own death and strong emotional reactions of loss to the death of loved ones. Viewing death as a loss and something to be feared, as opposed to a natural or tranquil transition, is often considered normal in the United States.
Source: https://courses.lumenlearning.com/boundless-psychology/chapter/aging-late-adulthood/
Posted by: schlinkwrign1989.blogspot.com
0 Response to "In What Culture Are Older People Sometimes Afforded Special Status"
Post a Comment